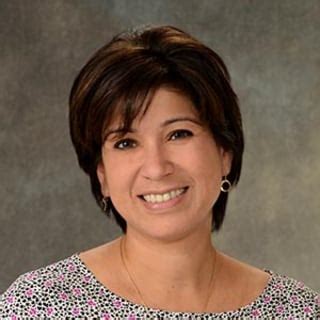
Dr. Cheryl Flynn, a renowned pain management specialist based in Rhode Island, has dedicated her career to alleviating pain and improving the quality of life for countless individuals. With a wealth of experience and an unwavering commitment to compassionate care, Dr. Flynn has emerged as a leading voice in the field of pain management.
Understanding the Burden of Pain
Pain is a ubiquitous experience that affects millions worldwide. According to the National Institutes of Health (NIH), chronic pain affects approximately 50 million American adults, costing the healthcare system billions of dollars annually. Pain can significantly impact an individual’s physical, emotional, and social well-being, leading to reduced mobility, depression, and even disability.
Dr. Flynn’s Approach to Pain Management
Dr. Flynn believes that effective pain management requires a comprehensive approach that addresses both the physical and psychological aspects of pain. She utilizes a holistic model that encompasses medication, physical therapy, cognitive-behavioral therapy, and lifestyle modifications.
Evidence-Based Treatments
Dr. Flynn employs evidence-based treatments that have been proven to reduce pain and improve function. These include:
- Opioid Management: Dr. Flynn carefully prescribes opioids when appropriate, utilizing guidelines to minimize potential risks.
- Non-Opioid Medications: She prescribes a range of non-opioid medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, and topical pain relievers.
- Physical Therapy: Dr. Flynn collaborates with physical therapists to develop personalized exercise programs that target pain sources and improve mobility.
- Cognitive-Behavioral Therapy: This therapy helps patients identify and modify negative thoughts and behaviors that contribute to pain perception.
- Lifestyle Modifications: Dr. Flynn encourages patients to adopt healthy habits, such as regular exercise, stress management techniques, and appropriate nutrition.
Customized Pain Management Plans
Dr. Flynn recognizes that every patient experiences pain differently. She tailors her treatment plans to each individual’s unique needs and preferences. By working closely with patients, she develops comprehensive pain management strategies that maximize outcomes.
Patient Education and Empowerment
Dr. Flynn believes that empowering patients is crucial for effective pain management. She provides extensive education on pain mechanisms, treatments, and self-management techniques. This knowledge enables patients to take an active role in their care and make informed decisions.
Advocacy and Research
Dr. Flynn is a passionate advocate for pain patients. She actively engages in research and policy discussions to promote improved pain care. She serves as a member of the Rhode Island Pain Task Force and has contributed to the development of state pain management guidelines.
Pain Points and Motivations
Pain Points:
- Chronic pain significantly impacts individuals’ quality of life, leading to reduced mobility, depression, and disability.
- Inadequate pain management can lead to reliance on ineffective treatments, such as abuse of alcohol or drugs.
- The high cost of chronic pain management places a financial burden on individuals and healthcare systems.
Motivations:
- Reducing pain intensity and improving function empowers individuals to live more active and fulfilling lives.
- Effective pain management promotes mental health by reducing depression and anxiety associated with chronic pain.
- Cost-effective pain care reduces healthcare expenditures and improves overall well-being.
Common Mistakes to Avoid
- Underestimating Pain: Dismissing or minimizing a patient’s pain can lead to inadequate treatment.
- Over-reliance on Medication: While opioids can be effective for acute pain, they should be used cautiously in chronic pain due to potential risks.
- Lack of Patient Education: Empowered patients make better decisions about their care. Providing comprehensive education is crucial.
- Ignoring Lifestyle Factors: Lifestyle modifications, such as exercise and stress management, play a significant role in pain management.
- Lack of Collaboration: Effective pain management requires collaboration between physicians, physical therapists, psychologists, and other healthcare professionals.
Frequently Asked Questions
1. What causes chronic pain?
Chronic pain can result from a variety of factors, including injuries, arthritis, nerve damage, and certain medical conditions.
2. How do I know if I need to see a pain management specialist?
If you have persistent pain that interferes with your daily activities and does not respond to over-the-counter medications, it is advisable to consult a pain management specialist.
3. What types of treatments are available for chronic pain?
Pain management treatments include medication, physical therapy, cognitive-behavioral therapy, nerve blocks, and surgical interventions.
4. Can I manage chronic pain on my own?
While self-management techniques, such as exercise and stress reduction, can help, chronic pain often requires professional intervention.
5. Is it possible to cure chronic pain?
While cure is not always achievable, effective pain management can significantly reduce pain intensity and improve function.
6. What are the risks of opioid use for chronic pain?
Opioids can be effective for acute pain but carry risks of addiction, misuse, and overdose when used long-term for chronic pain.
7. How can I prevent chronic pain from worsening?
Maintaining a healthy weight, engaging in regular exercise, and managing stress can help prevent chronic pain from progressing.
8. What is nerve damage pain?
Nerve damage pain, also known as neuropathic pain, is caused by damage to the nerves. It is characterized by burning, tingling, or shooting pain that is often difficult to treat.
Tables
Table 1: Prevalence of Chronic Pain in the United States
| Condition | Number of Affected Adults |
|---|---|
| Lower Back Pain | 27.3 million |
| Neck Pain | 15.1 million |
| Arthritis | 14.1 million |
| Headache | 13.2 million |
| Facial/Oral Pain | 10.8 million |
Table 2: Benefits of Comprehensive Pain Management
| Benefit | Description |
|---|---|
| Reduced Pain Intensity | Lowering pain severity levels |
| Improved Function | Increasing mobility, reducing disability |
| Enhanced Mood | Alleviating depression and anxiety |
| Improved Quality of Life | Increasing participation in activities and social engagements |
| Reduced Healthcare Costs | Minimizing hospitalizations and emergency room visits |
Table 3: Pain Relief Modalities
| Modality | Description |
|---|---|
| Medication | Prescribed drugs, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and antidepressants |
| Physical Therapy | Exercises, stretches, and therapeutic modalities to improve mobility and reduce pain |
| Cognitive-Behavioral Therapy | Techniques to manage negative thoughts and behaviors that contribute to pain perception |
| Nerve Blocks | Injections of local anesthetics or steroids to block pain signals from nerves |
| Surgery | Surgical procedures to repair or alleviate structural causes of pain |
Table 4: Lifestyle Modifications for Pain Management
| Modification | Description |
|---|---|
| Regular Exercise | Engaging in physical activity to strengthen muscles, improve flexibility, and reduce pain |
| Stress Management Techniques | Practicing mindfulness, yoga, deep breathing exercises, and meditation to minimize stress and anxiety |
| Healthy Nutrition | Consuming a balanced diet that includes plenty of fruits, vegetables, and whole grains |
| Sleep Hygiene | Establishing regular sleep patterns, creating a conducive sleep environment, and addressing underlying sleep disorders |
| Smoking Cessation | Quitting smoking, which can contribute to inflammation and pain |